Everything else
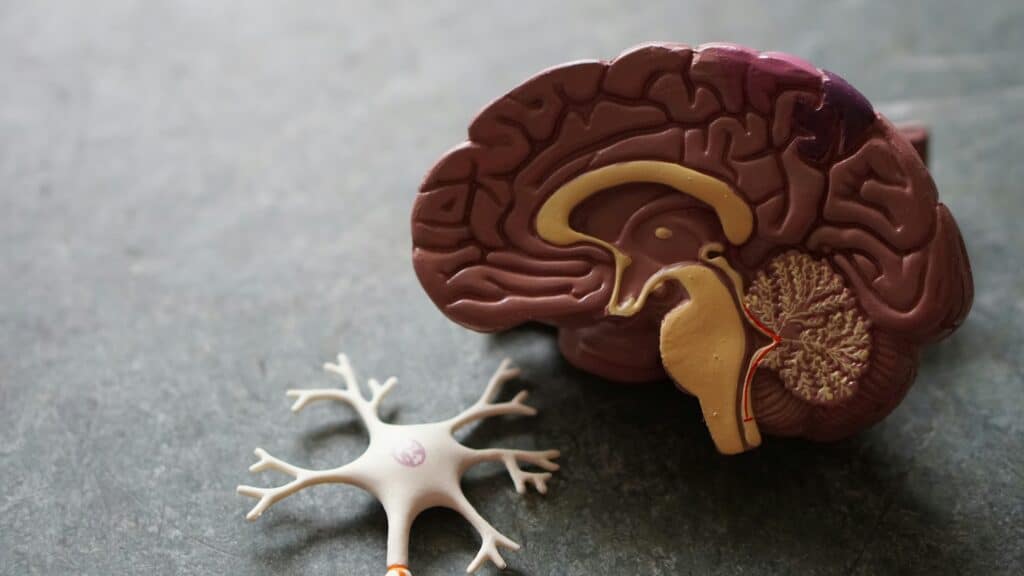
The Role of Your Mind In Your Health
Here is something curious I have noticed: people who are ultra-obsessed with their health (especially their diet) often seem to live sicker lives than people who are more balanced and carefree.
That is why the study I am about to discuss is absolutely no surprise to me. You will find this interesting. While this study is about gluten intolerance in particular, the principle applies to many health issues.
About the Study
A recent 7-day study of 28 irritable bowel syndrome (IBS) patients reveals a striking finding: belief matters more than actual gluten consumption when it comes to symptom flare-ups.
Participants, most with years of experience with a gluten-free diet, were given identical cereal bars during three separate periods. Some bars contained wheat and gluten (11 and 8.9 grams respectively), while control bars contained neither. Critically, participants didn’t know which bars contained gluten. Researchers measured changes in symptoms and asked participants to guess what was in each bar.
The Key Finding
IBS symptoms did not differ between participants who consumed wheat or gluten and those who consumed control bars. However, participants reported significantly worse symptoms when they believed they had eaten gluten or wheat—even when they actually hadn’t.
This dramatic gap between actual intake and perceived intake points to a powerful placebo effect.
One month after learning the results, only 12% of participants abandoned their gluten-free diet, suggesting long-standing beliefs were difficult to overturn even with scientific evidence.
Why This Matters
The results align with broader research showing that IBS, partially driven by abnormal gut-brain communication, is highly susceptible to psychological factors. In drug trials, roughly 27% of IBS patients improve on placebos, and over 30% experience adverse effects from placebos alone. This suggests beliefs genuinely influence symptoms through mind-body pathways.
The Broader Context
Many IBS patients adopt restrictive gluten-free diets based on perceived symptom improvements, but prior meta-analyses paint a similar picture: only about 16% of people with IBS show genuine gluten sensitivity. Meanwhile, 40% experienced similar or worse symptoms with placebos compared to actual gluten.
A 2024 study reinforced this by showing symptoms worsened primarily when participants knew they were consuming gluten, not from the gluten itself.
Clinical Implications
Restrictive diets carry real costs: reduced nutrient intake, poorer gut health, and diminished quality of life. Major medical organizations don’t recommend gluten-free diets for IBS patients without confirmed celiac disease or gluten sensitivity.
The Takeaway
This research suggests that for many IBS patients without celiac disease, symptom relief from gluten-free diets stems from belief rather than biology. Before committing to long-term dietary restrictions, the evidence supports conducting proper gluten challenge tests to determine whether gluten actually triggers symptoms, rather than relying on dubious diagnoses from professionals who don’t do legitimate testing.
Photo by Robina Weermeijer on Unsplash